Imagine a scenario where a medical device used in thousands of surgeries across the world starts showing signs of malfunction. Perhaps a defective component, undetected during manufacturing, begins to affect patient safety.
Tracing the device's origins—its materials, manufacturing process, and distribution history—could save countless lives. With traceability regulations in place, manufacturers can identify affected batches, initiate recalls, and prevent further harm. Without it, resolving the issue could take weeks or months, exposing patients to unnecessary risk and jeopardizing a company's reputation.
By building traceability into every stage of medical device manufacturing, companies can meet regulatory requirements and deliver safer, more reliable products to the market.
Let’s explore what traceability entails and how it shapes the manufacturing process.
Definition of Traceability in Medical Device Manufacturing
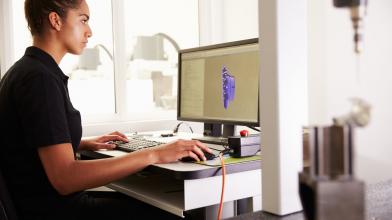
Traceability in medical device manufacturing refers to the systematic process of tracking and documenting a device's journey from conception to post-market use. This includes recording critical data such as raw material sourcing, production details, testing results, and distribution information.
The goal is to track each product throughout its lifecycle for quick identification of any quality issues. Traceability is vital for maintaining product safety, quality control, and adherence to global and regional standards.
Requiring traceability in medical device manufacturing helps manage risks and provides transparency for manufacturers, regulators, and patients, fostering accountability across the medical device supply chain.
ISO 13485 and Traceability: What They Mean for Medical Device Manufacturing
Traceability in medical device manufacturing is shaped by a combination of international standards and regional regulations.
ISO 13485 defines the global standard for quality management systems in medical device manufacturing and provides a framework to help organizations meet regulatory and safety requirements.
National regulations like the FDA's Unique Device Identification (UDI) system in the U.S. and the EU Medical Device Regulation (MDR) expand on this standard with specific traceability mandates in their respective regions. Other regions may have their own variations in traceability requirements, which can depend on factors such as device classification or local regulatory standards.
Understanding the distinctions in traceability requirements is essential for companies operating in multiple markets.
ISO 13485: The Foundation of Medical Device Traceability
ISO 13485, the global standard for quality management systems in medical devices, establishes the foundation for effective traceability.
It requires manufacturers to maintain clear documentation and records, ensuring accountability at every stage of the product lifecycle—vital for compliance and risk management for Class I, II, and III medical devices.
Key requirements related to traceability under ISO 13485 include:
Document Control Procedures
All documents related to the device are controlled and traceable, preventing the use of outdated or incorrect information.
Production Records
Detailed documentation of each step in the production process, tracking components and manufacturing methods used for every device.
Corrective and Preventive Action (CAPA) Systems
When quality issues arise, these systems require manufacturers to document the problem, investigate the root cause, and implement corrective actions to prevent recurrence.
FDA's Unique Device Identification (UDI) System
In the U.S., the FDA’s Unique Device Identification (UDI) system requires devices to include unique identifiers, such as batch numbers and expiration dates. These identifiers must be readable by humans and machines, enabling effective recalls or audits.
Unique device identification consists of two parts:
1. Device Identifier (DI): A unique code that identifies the device’s specific version or model.
2. Production Identifiers (PI): Information such as lot or batch number, serial number, manufacturing date, and expiration date, providing traceability for individual units.
These identifiers help medical device manufacturers and regulatory authorities quickly trace devices, enhancing patient safety during recalls and audits.
FDA Requirement for Written Standard Operating Procedures (SOPs)
The FDA mandates that medical device manufacturers establish written Standard Operating Procedures (SOPs) to aid compliance with quality assurance, tracking, and distribution processes.
Aspects of SOPs under FDA regulations include:
Production and Process Controls
Manufacturers must establish documented instructions and methods to control production processes, ensuring devices meet specifications and deviations are effectively managed and documented.
Monitoring and Control
SOPs must outline how production parameters, including device characteristics, are monitored and controlled to confirm consistent product quality.
Record-Keeping for Distribution
Detailed procedures for documenting the movement of devices from the manufacturer to distributors, healthcare providers, and patients must be included, supporting traceability and regulatory compliance during distribution.
These SOPs are essential for maintaining consistency and reducing errors in tracking and distribution, ultimately enhancing traceability, compliance, and patient safety.
EU Medical Device Regulation (MDR)
In Europe, the EU Medical Device Regulation (EU MDR) establishes strict traceability requirements and ongoing surveillance for most manufacturers and medical devices.
Some of the key traceability elements under EU MDR include:
Implantation of a UDI System
Similarly to the FDA, EU MDR requires unique identification of medical devices to strengthen traceability throughout their lifecycle.
Increased Emphasis on Post-Market Surveillance
Manufacturers are required to actively monitor device performance and safety post-market, collecting and analyzing data to detect potential issues.
Stricter Requirements for Clinical Data
The EU MDR mandates more precise clinical evidence to support the safety and efficacy of devices, further linking traceability with patient safety.
These requirements are embedded in the 10-step EU MDR’s compliance process, some of which include device classification, manufacturer registration, and fulfilling post-market obligations.
Effective Data Management for Traceability in Contract Manufacturing
Data management is the backbone of traceability in contract manufacturing. For medical devices, where safety and quality are paramount, maintaining organized, accessible records is critical to providing accountability at every stage of production.
Modern traceability relies on technologies that centralize and organize critical data, integrating it into a compliant data management system. These technologies include:
Barcodes and Data Matrices
Widely used for labelling medical devices, allowing quick identification and tracking. Two common formats in medical device labelling are:
1. Linear Barcodes: One-dimensional codes consisting of parallel lines and spaces of varying widths, suitable for encoding limited data like product codes.
2. 2D Data Matrix Codes: Two-dimensional codes consisting of black and white modules arranged in a square or rectangular pattern. They can store more information than linear barcodes, including product details, batch numbers, and expiration dates.
QR Codes and RFID Tags
Provide real-time tracking capabilities, especially for high-value or sensitive medical devices:
1. QR Codes (Quick Response Codes): Two-dimensional codes that can be scanned using smartphones and other devices, providing quick access to product information or linking to online resources.
2. RFID Tags (Radio-Frequency Identification): Radio waves are used to communicate with a reader, allowing for wireless tracking of devices without line-of-sight scanning.
Real-Time Location Systems (RTLS)
This is an emerging traceability technology in the medical device manufacturing space that offers precise monitoring of devices during storage and distribution. RTLS utilizes technologies like Wi-Fi, Bluetooth, or ultrasound to track device locations and environmental conditions.
By utilizing these tools, manufacturers create a unified data management system that enables regulatory compliance and bolsters accountability throughout the supply chain.
The Role of Data Management in Outsourced Manufacturing
Outsourced manufacturing introduces new complexities, requiring accurate data coordination between original equipment manufacturers (OEMs), contract manufacturers, and suppliers.
Effective data management addresses these challenges by:
Component Sourcing and Quality Tracking
Capturing supplier details, batch numbers, and quality certifications enhance transparency and traceability throughout the supply chain.
Production and Distribution Monitoring
Following production stages and device movement through distribution networks helps quickly identify quality issues, maintain traceability, and analyze adverse event trends.
By digitally recording these data points, manufacturers guarantee all parties have access to up-to-date and accurate information, critical for maintaining compliance and patient safety.
Benefits of Traceability in the Contract Manufacturing of Medical Devices
With traceability systems in place, companies working with contract manufacturers gain the following advantages that directly impact quality, transparency, and collaboration:
1. Enhanced Response to Quality Issues: Traceability allows manufacturers to identify and isolate defective batches, mitigating recall impact and strengthening trust between medical device manufacturers and patients.
2. Improved Supply Chain Transparency: Companies can monitor every aspect of their supply chain, from raw material sourcing to final product distribution. This transparency helps maintain consistent quality and collaboration with contract manufacturing partners.
3. Stronger Collaboration with Contract Manufacturers: OEMs and contract manufacturing partners can better align their operational processes when they have access to synchronized data. This facilitates stronger partnerships, reduces errors, and provides regulatory compliance.
Traceability is more than a regulatory requirement—it’s a strategic advantage for businesses in medical device manufacturing who invest in doing it the right way.
Choose an ISO 13485-Compliant Partner for Your Medical Device Manufacturing
Working with a contract manufacturer who prioritizes medical device traceability as a strategic asset—not just a checklist item—opens doors to better quality, deeper trust, and smoother operations.
Our ISO 13485-certified facilities are designed to protect and advance your business, giving you a clear advantage in an industry where precision and transparency define success.
Learn more about how we can support your medical device manufacturing goals by visiting our Medical Devices Manufacturing page.